Donald Downer, MD
Welcome to Clay Eye Physicians & Surgeons, where exceptional cornea care is led by our distinguished specialist, Donald Downer, MD. With his profound expertise in corneal disorders and innovative approaches to treatment, Dr. Downer is dedicated to restoring and preserving the clarity and health of your eyes. His commitment to patient-centered care ensures that you receive the highest level of attention and tailored solutions for your cornea-related concerns.
Corneal Conditions
Corneal conditions include a variety of conditions that affect mainly the cornea. These include infections, degenerations, and disorders that may arise mostly as a result of heredity. Some of the corneal conditions and treatment include:
• DRY EYE SYNDROME
• KERATOCONUS
• CONTACT LENS INFECTIONS
• CORNEAL TRANSPLANTATION (DSEK / PKP)
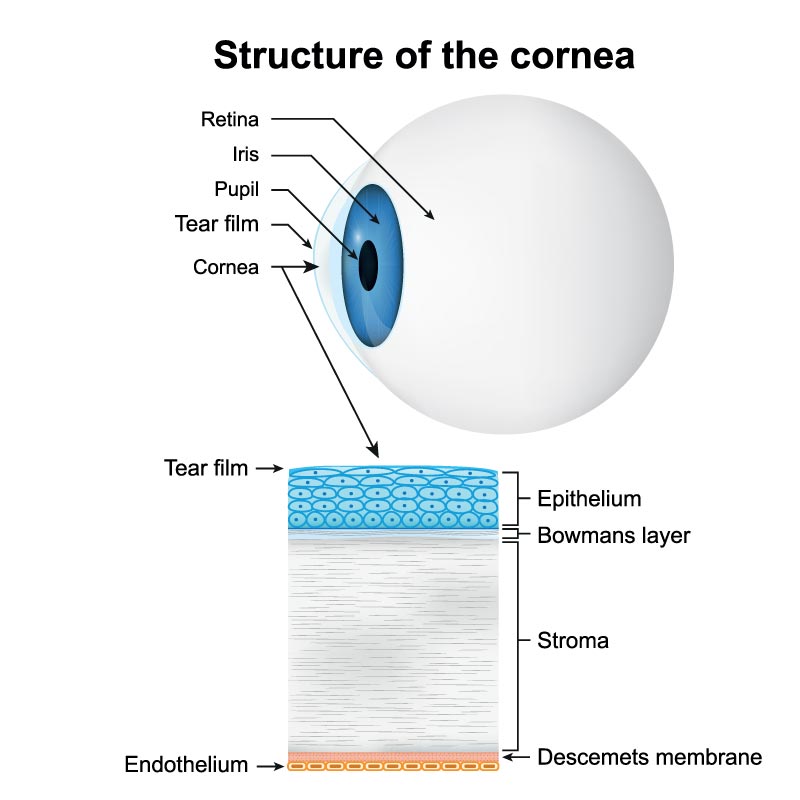
What is the Cornea?
The cornea is the clear, protective outer layer of the eye. It acts as a shield, protecting the eye from germs, dirt, and other particles that can harm the eye, and significantly contributes to the eye’s ability to focus.
The cornea is a lens that serves as the entry point for light into the eye and plays a significant role in overall vision. As light enters the eye, it is refracted, or bent, by the outside shape of the cornea. The curvature of this outer layer helps determine how well your eye can focus on objects both close up and far away. Although the cornea is surprisingly strong and durable, if the cornea becomes damaged through disease, infection, or injury, the resulting scars or discoloration can interfere with vision by blocking or distorting light as it enters the eye.
What are the symptoms of Corneal Conditions?
With its ability for a quick repair, the cornea usually heals after most injuries or disease. However, when there is a deep injury to the cornea, the healing process may be prolonged, possibly resulting in a variety of symptoms, including:
- Pain in the eye
- Blurred or reduced vision
- Tearing
- Redness or inflammation in the eye
- Extreme sensitivity to light
- Corneal scarring
- Headache, nausea, fatigue
If you experience any of the symptoms listed above, call our office to schedule an appointment. You may be experiencing a more serious problem and require immediate attention.
Dry Eye Syndrome
Dry Eye Syndrome is the lack of lubrication or moisture in the eyes related to the tear film and production of natural tears. This syndrome can be caused by factors including the natural aging process, cold medicines, contact lens wear, and certain environmental factors.
If you have a dry and scratchy feeling or a burning sensation, you may be experiencing dry eye. To determine if you are suffering from this syndrome, it is important to make an appointment with one of our dry eye specialists. During this appointment, a test called the Schirmer test will be conducted to determine the severity of the dryness in your eyes.
What causes dry eyes?
The exact cause of Dry Eye Syndrome is still being researched by the medical community, but it has been determined that certain elements are known to cause dry eyes. Certain diseases such as lupus, rheumatoid arthritis, or Sjögren’s Syndrome can cause dry eyes. Some prescription medications and over-the-counter medications can also lead to dry eyes, as well as contact lens wear, and environmental factors. Some medications that are known to cause dry eyes are antihistamines, such as Benadryl, some blood pressure medications and anti-depressants. Also, if you are a smoker, you are at risk for developing Dry Eye Syndrome.
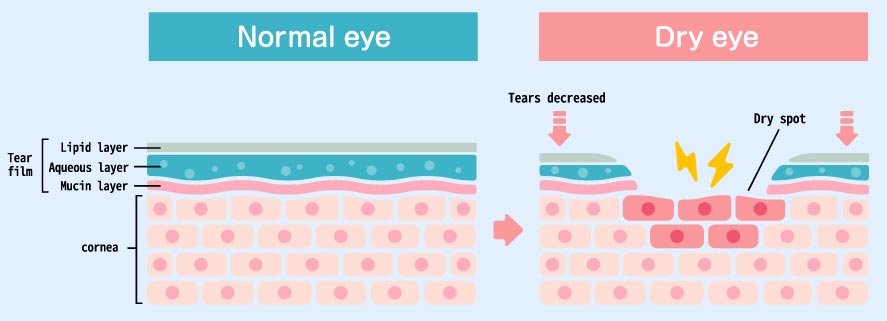
The Tear Film
The tear film is made up of three different layers: an oily layer, a watery layer, and a mucin layer. The small glands on the edge of the eyelid called meibomian glands, produce the oily layer of the tear film. The oily layer is what smooths the tear surface and decreases the evaporation of tears. The watery layer is the middle layer and the largest layer. The watery layer is produced by small glands on the conjunctiva which is the membrane lining the inside of the eyelid and covering the eyeball. The innermost layer is the mucus layer produced by goblet cells in the conjunctiva. This layer is what allows the watery layer to spread evenly over the surface of the eye and helps to keep the eye moist.
Treatment Options for Dry Eye
Dry Eye Syndrome is difficult to cure, but there are certain treatments to help reduce the effects including:
- Over the counter/Dry Eye drops: Certain over-the-counter drops can help relieve dry eyes in the short term. Artificial tears are available without a prescription and can be used as often as necessary for relief.
- Restasis: After a complete eye exam is conducted, and your physician assesses your individual situation, the prescription eye drop that might be a great option for you, could be Restasis.
- Flaxseed oil tablets or oil: Studies have shown that flaxseed oil can minimize the effects of Dry Eye Syndrome. It has been determined that ingesting the oil is better than taking the tablets because of how it is absorbed into your system.
- Punctal Plugs: These plugs are inserted to help with the natural tear flow.
- Nutraceuticals or dry eye vitamins: Certain vitamins have been shown to significantly help Dry Eye Syndrome. They are also a good source of other essential minerals. In most cases, consistent usage is required for results.
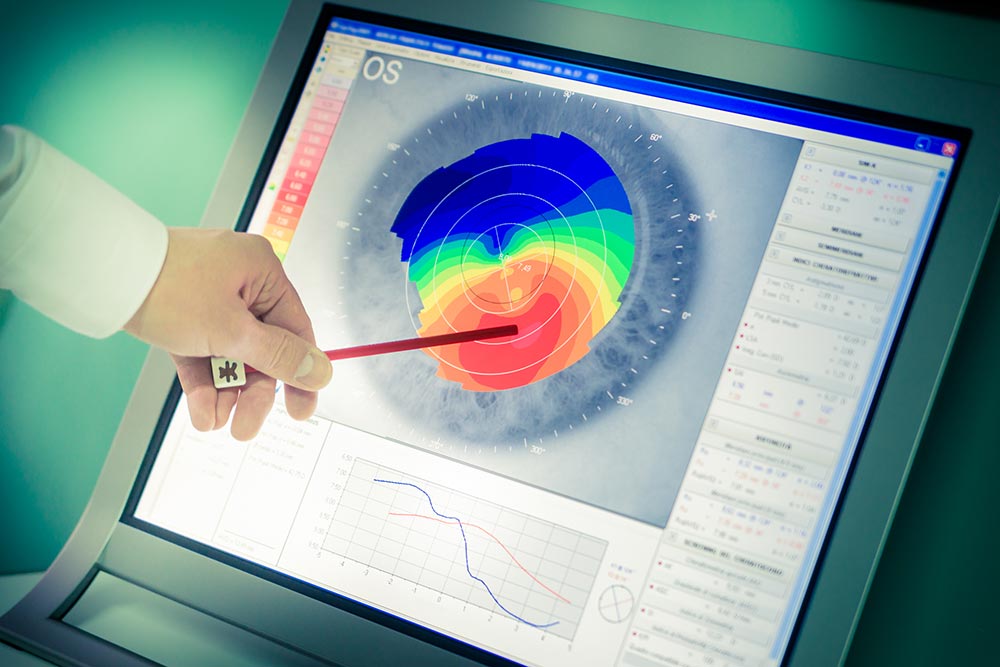
What is Keratoconus?
Keratoconus (KEHR-uh-toh-KOH-nus) is a very rare eye condition in which the normally round, dome-like cornea (the clear front window of the eye) becomes thin and develops a cone-like bulge. Keratoconus literally means “cone-shaped cornea.” Keratoconus is typically treated by a corneal specialists. A Corneal Specialist has done a specific Corneal Fellowship, with extensive training on the cornea and corneal diseases.
The cornea is a very important part of your eye. As light enters the eye it refracts or focuses, the light rays so that you can see clearly. With keratoconus, the shape of the cornea is altered distorting your vision. Keratoconus can make some activities such as driving, typing on a computer, watching television or reading very difficult.
What causes Keratoconus?
The cause of keratoconus is still unknown. However, it has been suggested that genetics may play a role in the development of keratoconus since 10% of those with the condition have an affected family member.
Symptoms of Keratoconus?
Keratoconus usually affects both eyes, however; symptoms in each eye may differ. Surprisingly, this is not an eye condition that affects only the elderly.
Symptoms usually start to occur in people who are in their late teens and early twenties and may include:
- A mild blurring of vision
- Distortion of vision
- Sensitivity to light
- Glare
- Slight irritation
How is Keratoconus treated?
Treatment of Keratoconus will often depend on the severity of the condition. During the early stages, vision can be corrected with eyeglasses. As the condition progresses, rigid contacts may need to be worn so that light entering the eye is refracted evenly and vision is not distorted. You should also refrain from rubbing your eyes as this can disrupt the thin corneal tissue and make symptoms worse.
In cases where contact lenses can no longer restore clear vision, cornea transplantation may be recommended. This surgery is only necessary for about 10-20% of patients with keratoconus. In a corneal transplant, a cornea specialist removes the diseased cornea from your eye and replaces it with a healthy donor cornea. While a corneal transplant will relieve the symptoms of keratoconus, it may not provide you with flawless vision; eyeglasses or contacts may still be needed to achieve your best vision.
Contact Lens Infections
Contact lens infections are on the rise as more and more patients look to replace their glasses with contact lenses. Despite the fact that many patients wear contact lenses daily, they do not realize that they can cause harm to their eyes if not cared for properly.
Contact lens infections can be caused by a variety of factors. They range from poor hygiene to an awkward fit. If you use contacts for vision correction or aesthetic purposes, your doctor will give you a prescription specific to your eyes.
One of the worst complications that contact wearers face is corneal ulcers. A corneal ulcer is an open sore in the outer layer of the cornea and is often caused by an infection. Germs such as viruses, bacteria, fungi or parasites are more likely to invade the eyes when contact lenses are worn for too long or are not cared for properly.
Poor contact lens hygiene, sleeping in contact lenses, and keeping lenses beyond their expiration date puts you at the greatest risks for these infections. Eye pain and redness are the earliest signs of an infection and require medical attention immediately. The most notable symptoms are redness, pain and sometimes discharge.
Antibiotics are effective for treating corneal ulcers, however they may not be effective immediately. On occasion, patients may have to spend time in the hospital. The worst scenario for a corneal ulcer is that partial to major vision may be lost.
Other Contact Lens Infections
A condition known as Giant Papillary Conjunctivitis (GPC) can occur as a reaction to contact lens use. The symptoms of GPC include mucus and itching of the eye. Once it has been determined that a patient suffers from GPC, contact lens use must stop immediately, so that treatment can be administered and your eye will have the ability to heal.
In cases where contact lenses can no longer restore clear vision, cornea transplantation may be recommended. This surgery is only necessary for about 10-20% of patients with keratoconus. In a corneal transplant, a cornea specialist removes the diseased cornea from your eye and replaces it with a healthy donor cornea. While a corneal transplant will relieve the symptoms of keratoconus, it may not provide you with flawless vision; eyeglasses or contacts may still be needed to achieve your best vision.
Practice Good Hygiene
We can not emphasize enough the importance of keeping your contacts clean. Wash your hands before inserting them and avoid any contact with a foreign surfaces when handling them.
Our Optometrists specialize in custom contact lens fitting. They conduct vision testing, measure your cornea and assess your overall eye health in order to find the best lenses specific to your eyes and your vision. It is their goal to help you select the best lenses to maximize both clear vision and overall comfort.
What is DSEK Eye Surgery?
If your cornea becomes cloudy, scarred or diseased, a corneal transplant could be your best option to save your sight. The cornea is a very important part of the eye, and, if left damaged, patients can suffer vision loss or blindness.
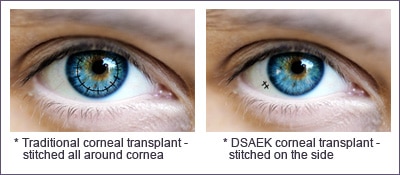
DSEK is a partial-thickness corneal transplant where a thin piece of donor tissue is inserted into the back surface of the patient’s cornea. This procedure helps patients who have corneas that are beginning to cloud over, due to endothelial dysfunction. The endothelium is the layer of pump cells on the back surface of the cornea. These cells pump fluid from the cornea to keep the tissue clear. If the pump cells are not working, the cornea will swell and become cloudy. With DSEK, instead of transplanting the full cornea, only the diseased pump cells are replaced.
Unlike a penetrating keratoplasty (PKP), which is a full-thickness corneal transplant where the donor tissue replaces the central cornea, DSEK uses a much smaller incision creating a smaller wound which is more stable and less likely to open with trauma.
Penetrating Keratoplasty (PK) Eye Surgery
If the entire cornea is unhealthy, then a full thickness corneal transplant, or penetrating keratoplasty (PK), may be necessary. Where the DSEK procedure is focused on transplanting only the endothelial cell layer of tissue, during a PK procedure a perfectly round circle of the cornea is removed from the patient and replaced with donor tissue. This new cornea is sutured into place with a stitch that is thinner than a human hair for a comfortable healing process.